Robotic prostatectomy, also known as robot-assisted radical prostatectomy, is a minimally invasive surgery for treating localised prostate cancer. With its precise instruments and advanced visualisation, robotic surgery has become a preferred choice for many patients seeking effective cancer treatment with reduced side effects.
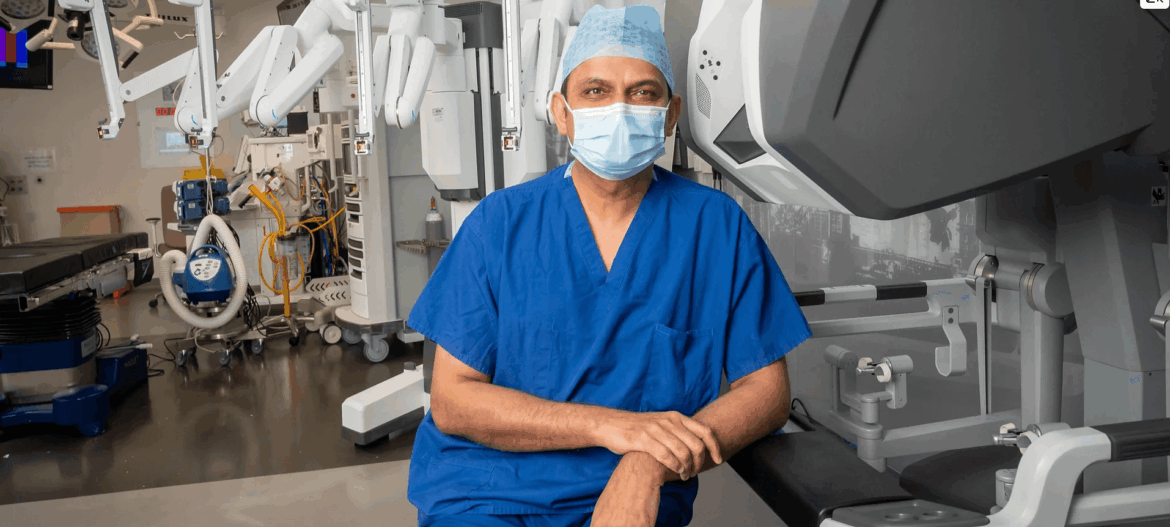
Professor Prokar Dasgupta uses state-of-the-art robotic techniques to achieve excellent outcomes in both cancer control and functional recovery.
Cancer Control Success Rates
Oncological outcomes are the primary measure of success for any prostatectomy. Key metrics include:
- Positive Surgical Margins (PSM): Low PSM rates indicate that cancer has been fully removed.
- Biochemical Recurrence: Monitored via PSA (prostate-specific antigen) testing; low recurrence rates show effective cancer control.
Studies indicate that robotic prostatectomy performed by experienced surgeons achieves cancer control rates comparable to, or even better than, traditional open surgery. In high-volume centers, over 90–95% of patients have clear margins, depending on tumor stage.
Urinary Continence Outcomes
Maintaining urinary control is a major goal of robotic prostatectomy. Recent data shows:
- Immediate continence: Some patients regain control soon after catheter removal.
- Continence within 3–6 months: Most patients achieve full continence within months.
Nerve-sparing approaches and minimally invasive techniques contribute significantly to faster recovery of bladder control.
Sexual Function and Erectile Outcomes
Preserving erectile function is another critical success measure. Key factors include:
- Use of nerve-sparing techniques, such as the SAFE method pioneered by Prof Dasgupta.
- Patient age, baseline erectile function, and tumor location.
Recent studies show that with bilateral nerve-sparing robotic prostatectomy, 50–70% of men may recover erectile function within 12 months, though individual outcomes vary.
Learn more about the SAFE nerve-sparing technique.
Factors That Influence Success Rates
Several factors affect outcomes:
- Surgeon Experience: High-volume surgeons have better cancer control and functional results.
- Patient Selection: Age, comorbidities, and baseline function impact recovery.
- Tumour Stage and Location: Advanced or aggressive tumours may limit nerve-sparing options.
- Technology and Technique: Innovations like robotic visualization, 3D planning, and SAFE nerve-sparing improve precision and outcomes.
Why Robotic Surgery Offers Advantages
Robotic prostatectomy allows:
- Enhanced 3D visualisation for precise dissection
- Tremor-free instrument control
- Smaller incisions with less blood loss
- Shorter hospital stay and faster recovery
- Better nerve-sparing potential
These advantages help explain why robotic surgery achieves high success rates in cancer control, urinary continence, and sexual function preservation.
Conclusion
The latest data confirms that robotic prostatectomy is highly effective, providing excellent cancer control while supporting functional recovery. With expert surgeons like Professor Prokar Dasgupta and advanced techniques such as SAFE nerve-sparing, patients benefit from improved outcomes, faster recovery, and minimised side effects.
For more information or to schedule a consultation, visit the Robotic Prostatectomy page on Prokar.co.uk.